Modern addiction’s impact on society extends far beyond individual struggles, costing the U.S. economy $2.7 trillion annually. You’ll find it manifesting through substance dependencies, digital obsessions, and mounting mental health challenges. Treatment gaps are widening, with only 6.3% of individuals receiving proper care, while healthcare provider shortages worsen accessibility issues. As addiction patterns evolve, particularly with digital dependencies affecting 56.9% of Americans, understanding these interconnected challenges reveals vital insights for traversing tomorrow’s health terrain.
The Hidden Economic Toll of Modern Addictions
The economic burden of addiction in modern society extends far beyond individual suffering, manifesting in a staggering $2.7 trillion annual cost to the U.S. economy equivalent to nearly 10% of the nation’s GDP.
You’ll find the most substantial impacts in direct financial losses, with alcohol ($249 billion) and illicit drugs ($193 billion) leading the charge. Fentanyl-related deaths alone account for $1.1 trillion, while productivity losses mount through increased unemployment rates among substance users. With 21.7 percent of Americans engaging in binge drinking, workplace efficiency faces significant challenges. Emergency departments face overwhelming pressure with over 630,000 visits annually related to alcohol abuse. Native American communities are disproportionately affected, experiencing substance use disorder rates nearly three times higher than other populations.
Recovery ecosystem fortification remains critically underfunded, with only 6.3% of individuals receiving necessary treatment. This treatment gap undermines societal investment prioritization efforts, as prevention costs pale in comparison to the astronomical price of inaction.
The strain extends across healthcare systems, criminal justice operations, and social services, creating a complex web of economic consequences.
Mental Health Crisis and Substance Dependencies
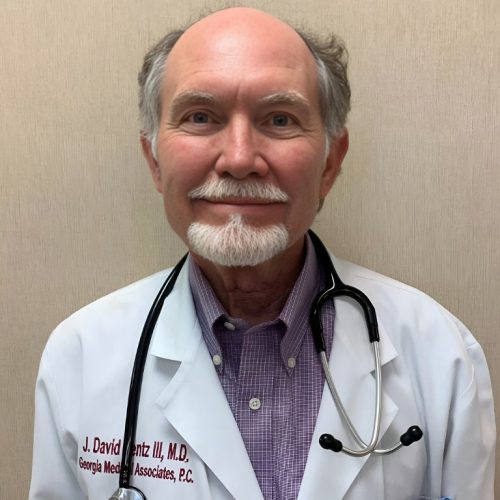
If you’re struggling with both mental illness and substance use disorders, you’re among the millions facing significant barriers to receiving integrated treatment, as only 6.3% of those with SUDs receive proper care.
Your chances of accessing thorough dual diagnosis treatment are further diminished by the projected shortage of 6,000 psychiatrists and 17,000 substance abuse providers by 2025.
The situation is especially concerning for young adults aged 18-25, where 24.4 percent face substance use disorders.
Recent data shows 105,007 Americans died from drug overdoses in 2023, highlighting the urgent need for expanded treatment access.
You’ll find these treatment gaps particularly pronounced in rural and low-income areas, where the scarcity of mental health professionals creates critical delays in accessing evidence-based interventions for co-occurring disorders.
Recent federal initiatives have prioritized Medicaid expansion funding to improve access to mental health and addiction treatment services nationwide.
Dual Diagnosis Treatment Gaps
Mounting evidence reveals a critical healthcare crisis at the intersection of substance use disorders (SUD) and mental health conditions, with recent data showing SUD prevalence doubling to 17.1% among Americans of all generations. You’ll find integrated care coordination severely lacking, as patients navigate fragmented systems while facing 15-20 year reductions in life expectancy. Primary care integration remains a significant challenge for SUD treatment providers seeking to improve patient outcomes. The emergence of virtual recovery platforms has created new opportunities for accessing dual diagnosis treatment remotely. Research demonstrates that patients with dual diagnosis require longer treatment periods compared to those with SUD alone.
| Treatment Barrier | Impact on Care |
|---|---|
| Stigma | 94.7% perceive no need for treatment |
| Access Gaps | Only 15% receive needed care |
| Clinical Training | Limited dual diagnosis expertise |
Medication assisted recovery models remain underutilized, particularly in rural areas where buprenorphine access is restricted. Current workforce limitations and structural inequities further compound these challenges, while housing instability creates additional barriers to sustained recovery. Amplified provider training and coordinated treatment pathways are urgently needed to address this growing crisis.
Mental Health Support Barriers
Recent analyses of mental health support barriers reveal a complex crisis at the intersection of workforce shortages and treatment access limitations. You’ll find cultural stigma and inadequate integrated care models significantly impacting treatment outcomes, particularly in underserved communities.
Critical challenges facing mental health support include:
- A projected shortage of 6,000+ psychiatrists by 2025, severely limiting professional care access
- Only 65% of adults with serious mental illness receiving necessary services
- Persistent racial and ethnic disparities in treatment accessibility, with rural areas facing severe resource gaps
- Limited implementation of integrated care models, with only 6.3% of individuals with substance use disorders receiving extensive treatment
These barriers disproportionately affect marginalized populations, highlighting the urgent need for systemic reforms and increased investment in mental health infrastructure.
Digital Age Dependencies: Beyond Traditional Substances

The digital revolution has spawned a new class of behavioral addictions that rival traditional substance dependencies in both prevalence and impact. You’re now part of a society where 56.9% of Americans acknowledge smartphone addiction, with the average person checking their device 144 times daily. This technology overuse manifests in concerning patterns: 71% of people prioritize screen time over partner interactions, while 44% experience separation anxiety from their devices. Research shows that check within minutes of waking up, demonstrating how deeply embedded these devices have become in daily routines.
The shift in the direction of electronic socialization has fundamentally altered relationships, with 85% of adults reporting near-constant internet usage. Your daily digital engagement likely reflects broader societal trends, where social media consumes 2 hours 22 minutes daily, and gaming addiction affects 105.6 million people worldwide. Studies show that teens spending 5+ hours on electronic devices are 71% more likely to exhibit suicide risk factors. Over a lifetime, social media usage alone can consume 5.7 years of an individual’s time. This unprecedented level of digital dependency presents unique challenges for maintaining healthy lifestyle balance.
Healthcare System Strain and Treatment Gaps
As healthcare systems buckle under unprecedented addiction-related demands, critical gaps in treatment infrastructure have emerged nationwide. You’ll find detox bed shortages and long term rehabilitation financing challenges creating severe bottlenecks in care delivery, particularly affecting marginalized communities.
Key systemic pressures include:
- Only 6.3% of individuals with substance use disorders received treatment in 2021, highlighting severe access limitations
- Healthcare costs now exceed $1 trillion annually, straining both institutional and patient resources
- 40-60% of treated patients experience relapse, indicating inadequate recovery support systems
- Treatment facilities face critical staffing shortages, especially in behavioral health specialties
These challenges disproportionately impact rural and underserved populations, where limited access to naloxone and specialized addiction services compounds the crisis. The rise in polydrug use involving methamphetamine and opioids has created additional complications for treatment providers. You’re witnessing a healthcare system struggling to adapt to synthetic opioids while managing increasing demand for evidence-based interventions. Recent data shows emergency department visits have surged by 99% due to opioid-related incidents, further straining hospital resources.
Social Fabric: Family and Community Impact

When you examine families affected by substance use disorders, you’ll find that trauma patterns often cascade through generations, with children being 8 times more likely to develop addiction themselves.
You’ll observe how addiction dismantles essential community support networks, leading affected families to withdraw from social connections and struggle to maintain healthy relationships.
The combination of intergenerational trauma and eroded social support creates a complex cycle that requires targeted intervention strategies to restore both family and community bonds. Research shows that family-based interventions are among the most effective prevention approaches for reducing substance use among young people, highlighting the importance of involving the entire family unit in recovery efforts.
Intergenerational Trauma Patterns
Intergenerational trauma patterns emerge through complex interactions between familial substance use, childhood adversity, and systemic inequities. You’ll find these transmission patterns particularly evident in families where substance use disorders persist across generations, creating cycles of trauma and addiction that require trauma-informed interventions to disrupt.
Key intergenerational impacts include:
- Children exposed to parental substance use show a 30% increased risk of developing addiction for each affected parent or grandparent
- Black women report family substance use at rates 5 times higher than other demographics
- Childhood trauma creates a direct pipeline to substance use disorder development by adolescence
- Environmental exposure in high-risk neighborhoods compounds family-based trauma effects
Understanding these patterns is essential for developing effective interventions that address both individual and systemic factors perpetuating the cycle.
Community Support Network Erosion
Modern communities face unprecedented challenges in maintaining social support networks for individuals struggling with substance use disorders. You’ll find that only 6.3% of affected individuals received treatment in 2021, highlighting a critical breakdown in community response systems. Parental support programs remain particularly underutilized, despite evidence showing children of addicted parents face four times the risk of developing substance use disorders.
| Impact Area | Current Gap | Solution Strategy |
|---|---|---|
| Family Support | 82% OUD cases untreated | Bolstered community outreach initiatives |
| Youth Services | 12.78% teen marijuana use | School-based prevention programs |
| Housing Security | 257,000 homeless with dual diagnosis | Housing-first + integrated care |
Community outreach initiatives must address these systemic failures, particularly in areas where genetic predisposition (40-60% of addiction risk) intersects with limited treatment access and inadequate support structures.
Criminal Justice System and Addiction Intersection
A vast majority of the American criminal justice system grapples with addiction-related challenges, as evidenced by the 85% of inmates who’ve active substance use disorders or addiction-linked criminal involvement. You’ll find probation integration challenges affecting 2.9 million people, while addiction driven crime reduction efforts show mixed results across jurisdictions.
Drug addiction plagues America’s justice system, with substance use disorders impacting 85% of inmates and millions under probation supervision.
The system’s scope is quantified through these key metrics:
- 171,300 individuals serve state prison sentences for drug-related crimes
- 1.16 million drug-related arrests occur annually
- 49,881 adults received substance treatment in secure settings (2023-2024)
- 38 states permit involuntary commitment for substance use treatment
Despite legislative shifts in the direction of treatment-based approaches, you’ll notice a persistent gap between clinical needs and available services, with many facilities lacking proper therapeutic environments for effective rehabilitation.
Workplace Productivity and Employment Challenges
While substance use disorders affect multiple aspects of society, their impact on workplace dynamics creates substantial economic and operational challenges. You’ll find that employees struggling with addiction show 20-30% decreased efficiency, leading to significant project coordination challenges and increased burnout risks for their colleagues.
| Impact Area | Key Effect |
|---|---|
| Productivity | 22+ annual absence days |
| Economics | $81B yearly U.S. losses |
| Team Dynamic | Trust/collaboration breakdown |
| Safety | Augmented accident rates |
| Healthcare | Rising insurance costs |
The workplace impact extends beyond individual performance, as substance use disorders create ripple effects throughout organizations. These include higher turnover rates, increased insurance premiums, and compromised safety protocols. Teams face disrupted workflows when managing substance-affected employees, often resulting in uneven workload distribution and heightened organizational stress levels.
Public Health Response and Prevention Strategies
Building upon workplace challenges, public health systems have implemented extensive response frameworks to address substance use disorders at societal levels. Through cross sector collaboration and data driven monitoring, you’ll find holistic strategies targeting prevention, treatment, and recovery.
Key public health initiatives include:
- SAMHSA’s 2025 National Guidelines establishing coordinated crisis care systems with emphasis on equity and accessibility
- CDC’s integrated approach to expanding medications for opioid use disorder while reducing healthcare disparities
- Technology-enhanced prevention strategies utilizing telehealth and digital platforms to improve service delivery
- Community-based harm reduction programs supported by $10 million in funding through SAMHSA’s FY 2025 budget
These evidence-based interventions demonstrate the public health sector’s commitment to systematic, measurable approaches in addressing substance use disorders across communities.
Policy Reform and Treatment Access
Recent policy reforms have transformed addiction treatment accessibility, driven by compelling evidence that only 6.3% of 46.3 million Americans with substance use disorders received care in 2021. You’ll find expanded medication subsidies addressing cost barriers while provider incentives bolster workforce capacity in underserved areas.
| Reform Area | Impact | 2025 Target |
|---|---|---|
| Medication Access | Increased naloxone distribution | 90% coverage |
| Provider Networks | Amplified MAT availability | Double providers |
| Insurance Coverage | Reduced treatment costs | Universal access |
Your treatment options now include federally supported programs targeting geographic disparities and removing financial obstacles. Data-sharing agreements between agencies enable better tracking of outcomes, while public-private partnerships fund community-based services. These reforms reflect strong public support, with 90% of Americans favoring local treatment centers and expanded access to evidence-based care.
Future Trends and Emerging Concerns
Despite recent declines in extensive overdose deaths, emerging synthetic drug trends and economic pressures pose unprecedented challenges for addiction treatment. You’ll need to understand how novel psychoactive substances and demographic trends in synthetic drug use are reshaping intervention strategies.
Key emerging concerns include:
- Rising prevalence of fentanyl-laced counterfeit pills, creating unprecedented overdose risks across all user demographics
- Shifting patterns of substance use among younger adults, particularly in the direction of synthetic drugs and social media-facilitated distribution
- Economic stressors driving increased addiction vulnerability, with treatment costs escalating due to synthetic drug complexity
- Post-pandemic behavioral health patterns revealing persistent comorbidity between substance use and mental health disorders
These trends suggest a critical need for adaptive treatment approaches and improved monitoring of emerging synthetic compounds.
Frequently Asked Questions
How Do Genetic Factors Influence Addiction Susceptibility Across Different Ethnic Groups?
Your genetic predisposition factors markedly influence addiction susceptibility, with variations across ethnic groups. You’ll find specific markers like ADH2 and ALDH2 variants in Asian populations affecting alcohol metabolism, while American Indian communities show distinct patterns in GABRA2/B1 clusters.
Cultural influences on addiction interact with these genetic components, creating unique risk profiles. You’re looking at heritability rates of 40-70%, though environmental factors still play an essential role in addiction development.
What Role Do Childhood Experiences Play in Developing Addiction Resistance?
Your childhood experiences profoundly shape your addiction resistance through multiple pathways. When you experience positive childhood mentorship and stable environments, you develop stronger emotional regulation and coping mechanisms.
Trauma healing plays a pivotal role, as unresolved adverse childhood experiences (ACEs) can increase your vulnerability to addiction. You’ll build greater resilience through supportive relationships and interventions that address early trauma, directly strengthening your natural defenses against substance dependence.
Can Alternative Medicine Approaches Effectively Support Traditional Addiction Treatment Methods?
Alternative medicine can effectively complement your traditional addiction treatment when properly integrated. Research shows that mindfulness meditation reduces cravings and stress by 40-60%, while targeted nutritional supplements help restore neurotransmitter balance.
You’ll find these approaches work best alongside evidence-based treatments, not as replacements. Studies indicate combining holistic methods with conventional therapy improves your recovery outcomes by up to 65% compared to single-modality approaches.
How Do Seasonal Patterns and Weather Conditions Affect Addiction Rates?
You’ll notice significant fluctuations in addiction rates that correlate with changing weather conditions throughout the year. During winter months, you’re more likely to see increased substance use due to seasonal depression (SAD) and disrupted circadian rhythms.
When daylight decreases, you experience lower serotonin levels, which can trigger drug-seeking behaviors. You’ll also face heightened risks during winter isolation, as limited social support and indoor confinement often lead to increased substance use as a coping mechanism.
What Impact Does Pet Ownership Have on Addiction Recovery Success?
You’ll find significant benefits from pet ownership during addiction recovery. Research shows that animal assisted therapy programs can augment your stress hormones while increasing feel-good chemicals like oxytocin and serotonin.
Pet socialization benefits include amplified emotional support, structured daily routines, and increased physical activity. Your recovery success rates improve through reduced isolation, consistent companionship, and the development of caregiving responsibilities. These factors contribute to a 31% lower risk of relapse.